Does Medicare Cover Colonoscopies in 2025?
If you’re deemed a high risk for colorectal cancer, then Medicare will cover the full cost of colonoscopy screenings once every two years. For patients who aren’t at high risk, Medicare will still cover screenings every 10 years.
In this article, I’ll review Medicare’s coverage for colonoscopies and whether other types of colon cancer screenings are included.
Medicare Colonoscopy Coverage
Colorectal cancer is the third most common cancer in the U.S. This is why it’s important to get screened. It’s recommended that people over the age of 50 get a colonoscopy every 10 years — particularly those with a family history of colorectal cancer. Although colorectal cancer affects all age and racial and ethnic groups, it most commonly affects individuals that are ages 50 and up, with the risk increasing with age.
According to the Centers for Medicare & Medicaid Services, those who are at high risk for developing colorectal cancer have the following factors:
- Close relative (sibling, parent, or child) who has had colorectal cancer or an adenomatous polyp
- Family history of familial adenomatous polyposis
- Family history of hereditary nonpolyposis colorectal cancer
- Personal history of adenomatous polyps
- Personal history of colorectal cancer
- Personal history of inflammatory bowel disease, including Crohn’s Disease and ulcerative coliti
In general, Medicare pays for the full cost of colonoscopy screenings if you’re high risk, so you don’t have to worry about the Part B deductible. However, there may be limitations to this, so check with your plan to see if there are any additional costs. For instance, if there is a polyp or abnormal tissue that’s found and removed during a colonoscopy, then there’s a good chance you’ll need to pay 20 percent of the Medicare-approved amount of your doctor’s services, including your copayment.
With no age limit, Medicare will cover colonoscopy screenings once every two years if you’re at high risk for colorectal cancer and have a family history of colon cancer. Alternatively, if you are not at high risk, Medicare will cover the test for you once every 120 months or 48 months.
Medicare Part A
Medicare Part A may pay for costs related to inpatient care for a colonoscopy in a hospital setting. You might need to pay a copay or a deductible, but for the most part, Medicare should cover the full cost.
Medicare Part B
Medicare Part B, or Medical Insurance, will cover a colonoscopy whether it’s for diagnostic or preventative purposes. You don’t need to meet your Part B deductible before Medicare coverage for the colonoscopy kicks in. However, you’ll be responsible for paying 20 percent for additional services such as the removal of polyps or other tissue.
Medicare Part C
Also known as Medicare Advantage, Medicare Part C helps cover colonoscopy screenings and provides additional benefits and assistance for out-of-pocket costs that aren’t typically covered by original Medicare. Keep in mind that Medicare Advantage plans are mandated by federal law to cover colonoscopy screenings. To avoid out-of-pocket costs, check to see if your provider is in network.
Medicare Part D
In terms of prescriptions, you might want to check to see what types of prescriptions are covered before and after undergoing a colonoscopy.
Medigap
Medigap covers certain gaps in coverage. You might want to check with your plan provider to see whether certain out-of-pocket costs can be covered.
Did You Know: Private insurance companies offer Medigap plans to help cover certain gaps in Medicare. Read my guide to Medicare Supplement Insurance to learn the benefits and cost savings of Medigap.
Cost of a Colonoscopy With Medicare
Ideal for older individuals who struggle with balance, mobility, or pain, lift chairs can help those with trouble sitting or standing up. They’re especially helpful for those with muscle or joint disorders and people recuperating from surgeries.
| Average cost of a colonoscopy | Medicare coverage | Out-of-pocket cost | Deductible | Total cost |
|---|---|---|---|---|
| $1,293 | $1,035 | 20% | N/A | $258 |
On average, a colonoscopy costs an average of $3,081 without health insurance. Fortunately, Medicare can cover the cost of colonoscopy screenings if you’re at high risk for colorectal cancer or other cancers.
In this hypothetical, let’s say Mary needs a colonoscopy and Medicare will be paying for most of the cost — with the exception of additional services such as the removal of a tumor or polyp. Because she needs a polyp and a lesion removed, she will have to pay 20 percent of the cost of these additional services. Medicare will cover 80 percent of the Medicare-approved amount for the colonoscopy and hospital stay fees, including anesthesia, which is covered by Medicare Part B.
Under Medicare’s procedure price lookup tool, Mary finds that she will need to pay on average $258 in out-out-pocket costs for hospital outpatient departments. The Medicare-approved amount that will be paid by Medicare will be $1,035 of the $1,293 total cost (this includes the doctor fee and facility fee). Fortunately, the yearly deductible does not have to be met for Medicare coverage to kick in to cover the colonoscopy and hospital stay. However, this doesn’t include the cost of other out-of-pocket costs such as aftercare following a colonoscopy, which might not be covered by Medicare or her plan.
Medicare Advantage and Colonoscopies
Medicare Advantage operates through private insurance companies. Plans may vary, so it’s best to reach out to your Medicare Advantage plan to see whether copays, deductibles, and other out-of-pocket costs are required. In general, Medicare will pay for patients who are at high risk for colorectal cancer or have a family history or other criteria that their physician can attest to.
Although Medicare can pay for the full cost of a colonoscopy provided certain criteria are met, there are exceptions. For instance, if there’s other tissue or a polyp that needs to be removed during a colonoscopy, the patient would be responsible for 20 percent of the cost, while Medicare would take care of the remaining 80 percent.
Medigap and Colonoscopies
Medicare supplement plans such as Medigap can help cover colonoscopies and other out-of-pocket costs. Fortunately, you don’t have to meet the deductible for Medicare Part B. The exception is if polyps or other tissue must be removed; then you’d be responsible for paying additional costs since it’s not covered by Medicare. It’s best to contact your Medigap plan first if your physician suspects that additional tissues may need to be removed, in addition to the colonoscopy, as these services may not be fully covered.
Does Medicare Cover Other Colon Cancer Screenings?
Medicare covers colorectal cancer screening tests targeting patients that are 50 and older. In general, there is no minimum age limit. Different parts of Medicare (A, B, and D) will cover some or all of the cost of colorectal cancer screenings and other services, pending certain criteria.
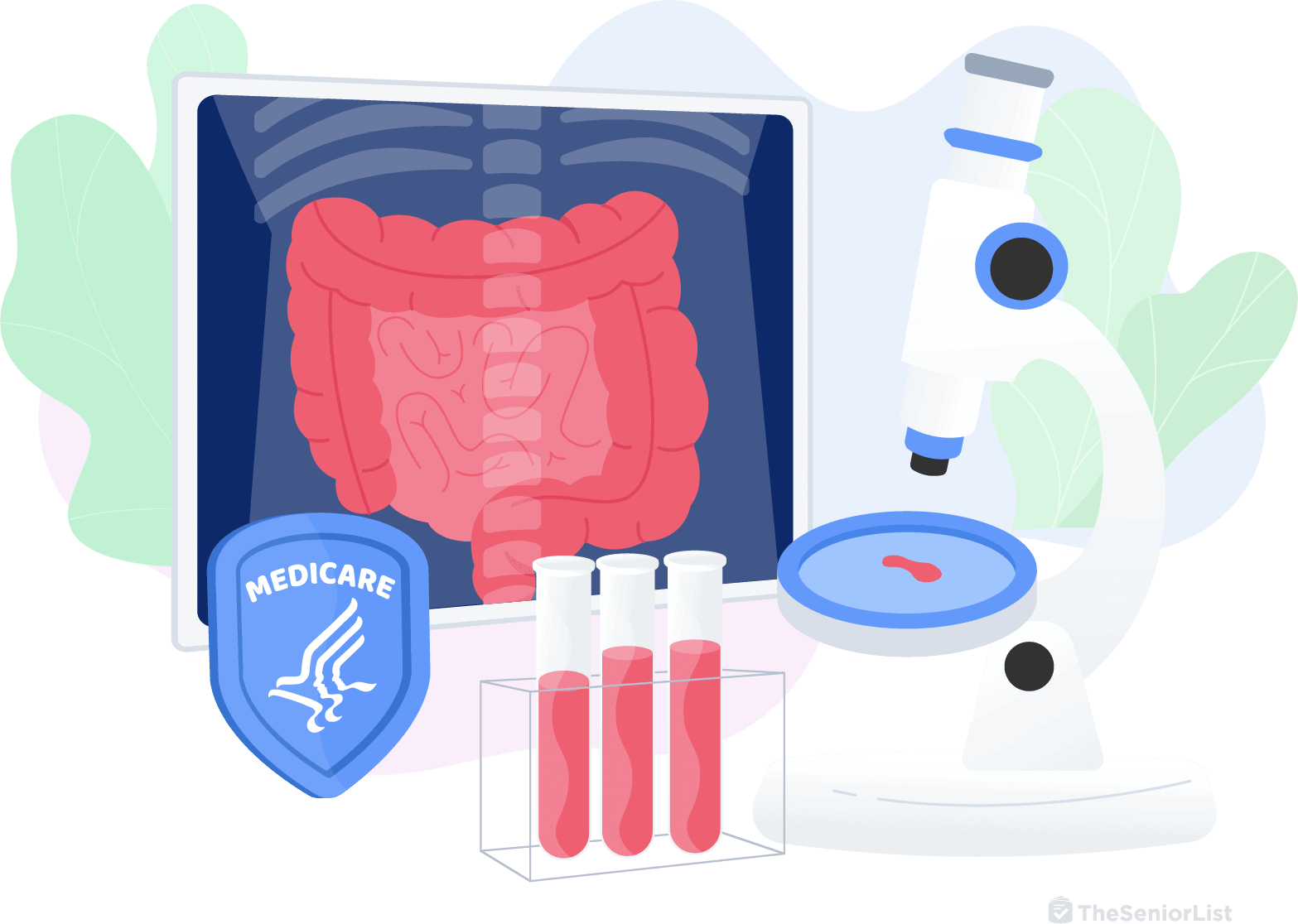
According to the Centers for Medicare & Medicaid Services, colorectal cancer screening can be done through a variety of tests, such as a fecal blood test, DNA test, and colonoscopy. For instance, Medicare Part B is responsible for covering the cost of the following different screenings for colorectal or colon cancer:
- Screening fecal occult blood test: Once every 12 months for people 50 or older
- Screening flexible sigmoidoscopy: Once every 48 months after the last flexible sigmoidoscopy or barium enema, or 120 months after a previous screening colonoscopy
- Screening colonoscopy: Once every 120 months (high risk, every 24 months), or 48 months after a previous flexible sigmoidoscopy
- Screening barium enema: Once every 48 months (high risk, every 24 months) when used instead of sigmoidoscopy or colonoscopy
- Multi-target stool DNA test: Once every 36 months if you meet certain conditions
These screenings are fully covered by Medicare if you receive a written referral from your physician or nurse practitioner and meet certain criteria. So if you have Medicare and need a flexible sigmoidoscopy or screening colonoscopy, you pay $0 if your physician accepts and approves the procedure. This means Medicare pays the full cost of fecal occult blood tests, flexible sigmoidoscopies, and colonoscopies, and you don’t have to worry about deductibles.
However, if during a colonoscopy, your physician needs to remove a tissue or a polyp, you may need to pay 20 percent of the Medicare-approved amount. Also, for barium enema screenings, Medicare can cover 80 percent, but you’d be responsible for 20 percent of the Medicare-approved amount, minus the Part B deductible. Additionally, if the barium enema screening is done in a hospital outpatient setting, you may need to pay a copayment and other fees, but it’s best to check with your plan for the latest figures.
Conclusion
With no minimum age requirement, Medicare covers colonoscopies every 24 months as long as your physician can certify that you’re at high risk for colorectal cancer. While Medicare can’t cover the cost of additional services such as the removal of polyps and other tissues, out-of-pocket expenses are still significantly reduced.
Medicare and Colonoscopies Frequently Asked Questions
-
Does Medicare cover the complete cost of a colonoscopy?
Medicare will cover the complete cost of a colonoscopy if the procedure is preventative and not diagnostic. If your physician needs to remove polyps or additional tissues, then Medicare will cover only 80 percent of Medicare-approved costs. Otherwise, it will cover the complete cost of a general colonoscopy.
-
Does Medicare require prior authorization for a colonoscopy?
Yes, Medicare requires prior authorization for a colonoscopy. Coverage will apply only if your physician authorizes a colonoscopy for the Medicare-approved amount.
-
How much does a colonoscopy cost out of pocket?
Typically, a colonoscopy costs between $1,250 and $4,000 out of pocket.
-
Will Medicare pay for a colonoscopy after age 80?
Medicare will pay for a colonoscopy for patients who are at high risk for colorectal cancer — regardless of age — every two years, and once every 10 years for those who are not at high risk.
-
Will Medicare pay for anesthesia for a colonoscopy?
Yes, anesthesia for a colonoscopy is covered by Medicare.